| Type | Cases | Deaths | DALYs |
|---|---|---|---|
| HAP (pneumonia) | 106,586 | 3,968 | 69,508 |
| SSI (surgical site) | 93,222 | 2,328 | 28,842 |
| BSI (bloodstream) | 26,976 | 3,905 | 58,350 |
| UTI (urinary tract) | 214,150 | 3,664 | 66,701 |
| CDI (C. difficile) | 36,002 | 1,917 | 20,890 |
| Total (all HAIs) | 478,222 | 16,245 | 248,920 |
Healthcare-associated infections (HAIs) are a major global health issue, associated with increased morbidity, mortality, and rising healthcare costs. Estimates suggest that 20–30% of HAIs in Germany could be prevented through improved hygiene and clinical procedures.
This post summarises Germany’s HAI burden (incidence, deaths, and disability-adjusted life years; DALYs) for five common HAIs: healthcare-associated Clostridioides difficile infection (CDI), healthcare-associated pneumonia (HAP), healthcare-associated primary bloodstream infections (BSI), healthcare-associated urinary tract infections (UTI), and surgical site infections (SSI) in 2011 and compares it with the EU/EEA average, using results from Zacher et al. (2019).
Methodology
The estimates come from the ECDC Point Prevalence Survey (PPS) of HAIs (2011–2012), covering 46 representative hospitals in Germany, 1,149 hospitals across 29 EU/EEA countries, and Croatia.
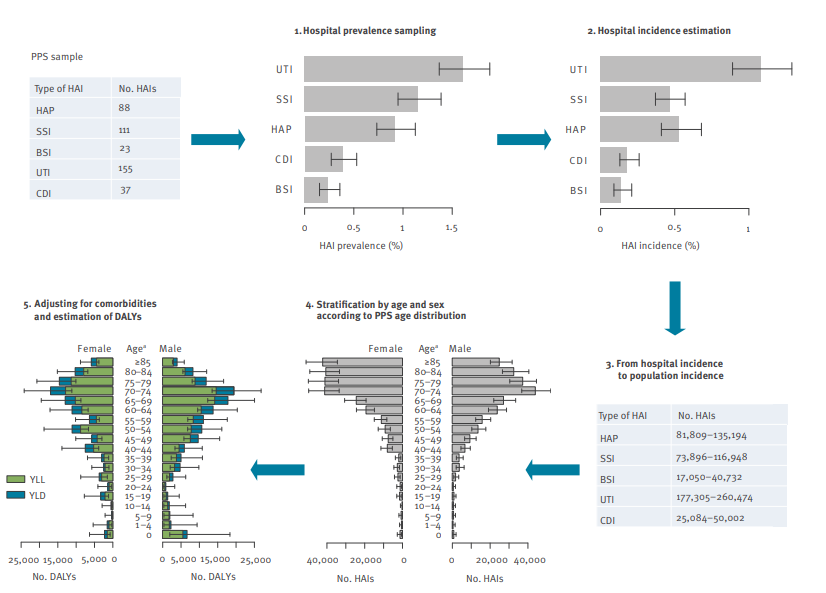
All calculations were implemented in the BHAI R package, which performs a predefined number of Monte Carlo simulations. The workflow (Figure 1) consisted of five main steps:
- Estimate hospital prevalence of HAIs from PPS data.
- Convert prevalence to hospital incidence using a modified Rhame–Sudderth formula and length-of-infection adjustments.
- Extrapolate incidence to the population level using hospital discharge data in Germany.
- Stratify by age and sex to reflect different life expectancies.
- Adjust for different life expectancies using McCabe scores, outcome trees, and Monte Carlo simulations.
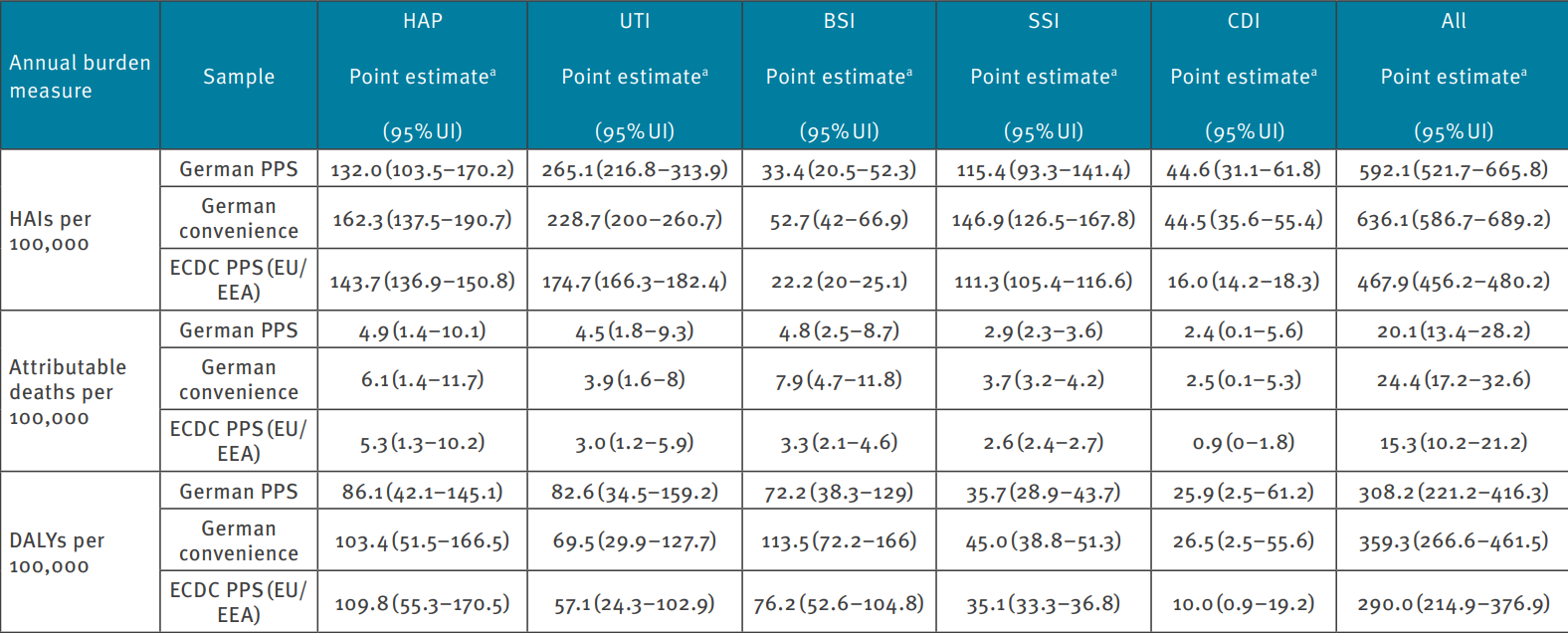
Using BHAI, the team estimated about 478,200 HAI cases in Germany in a single year — leading to 16,200 attributable deaths and a total of 248,900 disability-adjusted life years (DALYs).
Table 1 summarises how different infection types contributed to the total burden.
These estimates form the basis for the following sections, which explore Germany’s overall burden, infection types, and demographic patterns.
Overall burden trends
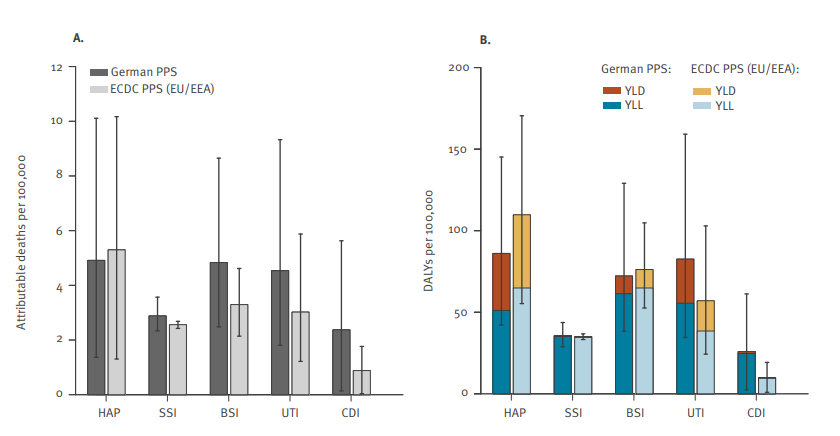
As shown in Figure 2, while Germany had a lower infection rate inside hospitals than the European Union average, its overall population burden was higher — 308 DALYs per 100 000 people, compared with 290 DALYs per 100 000 across the EU/EEA. This indicates that Germany experiences a high burden.
This national overview provides the big picture. To understand where these numbers come from, we can look closer at how different infection types contribute to the total burden.
Detailed comparison across infection types
While Figure 2 shows the overall pattern, the numerical estimates in Figure 3 break down the burden by infection type. Germany’s infection rates and burden indicators were consistently higher than those of the EU/EEA across all five infections. The annual population incidence reached 592 per 100 000 in Germany versus 468 per 100 000 in the EU/EEA. Similarly, attributable deaths were 20.1 vs 15.3 per 100 000, and DALYs 308 vs 290 per 100 000.
Among infection types, pneumonia (HAP) and bloodstream infections (BSI) accounted for most of the difference, driven by their higher fatality rates. By contrast, urinary tract infections (UTIs) were more frequent but caused a smaller share of DALYs, while C. difficile infections (CDI), though rarer, still added a notable contribution.
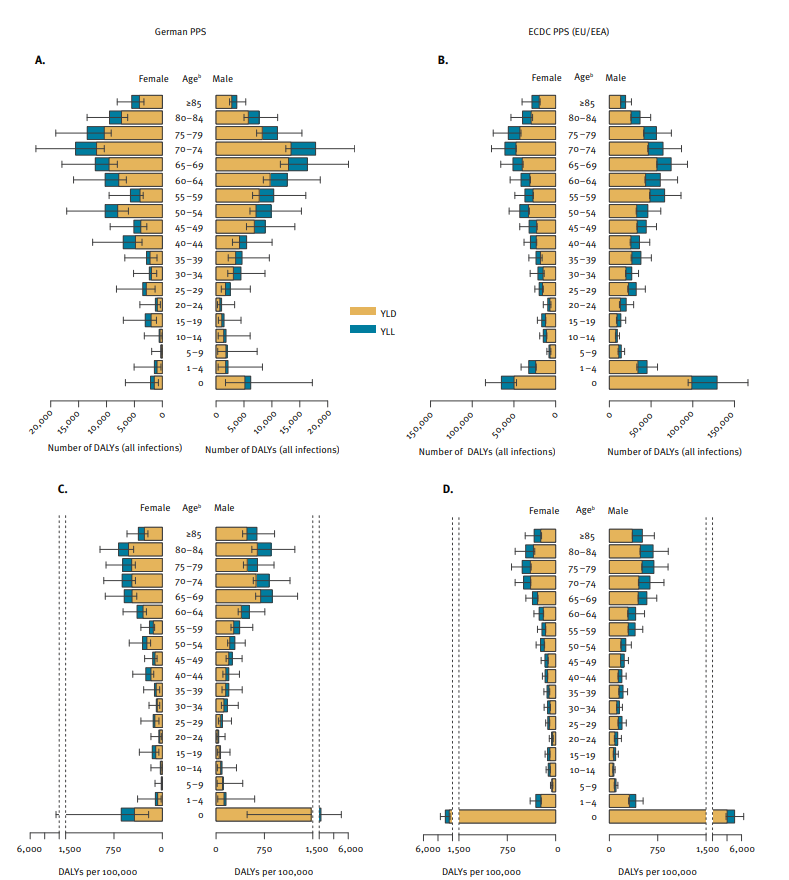
Burden by Age and Gender
Beyond infection type, demographic factors also shape the burden. As shown in Figure 4, DALYs increase sharply with age, peaking among adults aged 75–84 years. Older age groups carry the majority of total health loss, reflecting their higher hospitalisation rates and vulnerability to severe outcomes.
Gender differences are smaller but consistent: across most age groups, men experience higher DALYs per 100 000 population than women. This likely reflects higher comorbidity and disease severity among men, while women’s longer life expectancy and greater representation in long-term care explain the small reversal seen at the oldest ages.
Germany’s ageing population amplifies these effects, helping explain why its population-level burden remains above the EU/EEA average even when hospital infection rates are comparable.
Why is Germany’s burden above the EU/EEA average?
These results raise a key question: if infection rates are low, why is the burden still higher?
Germany has one of the highest hospital admission rates and the largest number of acute care beds in Europe. This means more people are exposed to potential infections — even if hospitals themselves perform well on hygiene standards.1
To reduce this burden, researchers recommend:
- Reducing avoidable hospital stays
- Focusing further on hygiene measures
- Enhancing infection prevention and control
In conclusion, Germany’s experience shows that reducing hospital use can be as powerful as improving hygiene — and the open-source BHAI tool makes such insights measurable for every country. As up to 30% of HAIs are preventable, these findings highlight how data-driven methods can guide smarter prevention strategies across Europe.
Reference:
Zacher B, Haller S, Willrich N, et al. Application of a new methodology and R package reveals a high burden of healthcare-associated infections (HAI) in Germany compared to the average in the European Union/European Economic Area, 2011 to 2012. Euro Surveill. 2019;24(46):1900135. https://doi.org/10.2807/1560-7917.ES.2019.24.46.1900135
Footnotes
These estimates should be interpreted with caution, as they rely on outcome trees informed by limited evidence, and on European McCabe score distributions, which may underestimate the German burden.↩︎